What is endometriosis?
Endometriosis occurs when tissue similar to the tissue that lines the uterus grows outside the uterus. This painful disorder affects about 10% of American women ages 15 to 44 and is especially common among those in their 30s and 40s, according to the Office on Women’s Health (OWH).
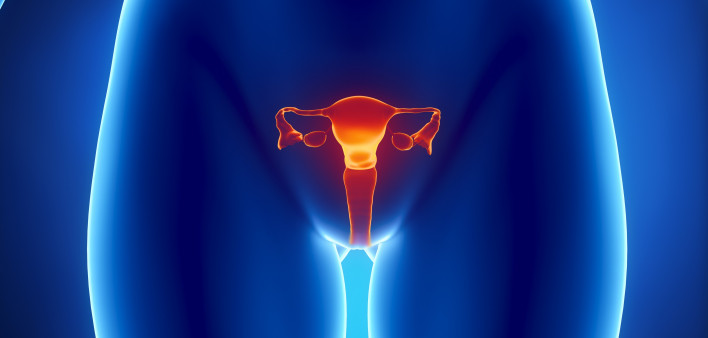
Endometriosis involves a woman’s ovaries, fallopian tubes and the tissue lining her pelvis. In rare cases, endometrial tissue may spread beyond the pelvic organs. Endometriosis makes it harder for women to conceive.
With endometriosis, the endometrial-like tissue that thickens, breaks down and bleeds with each menstrual cycle is unable to exit the body and becomes trapped. When the ovaries are involved, cysts called endometriomas form, causing the tissue to become irritated and sometimes develop into scar tissue and adhesions.
What are the symptoms of endometriosis?
According to the OWH, pain is the most common symptom women with endometriosis experience. The different kinds of pain include:
- Very painful menstrual cramps with pain that may worsen over time
- Chronic (long-term) pain in the lower back and pelvis
- Pain during or after sex that’s usually described as a “deep” pain. This pain differs from the pain that may be felt at the entrance to the vagina upon penetration.
- Intestinal pain
- Painful bowel movements or pain when urinating during menstrual periods. In rare cases, blood may be found in a woman’s stool or urine.
Other symptoms are:
- Bleeding or spotting between menstrual periods. However, this can be caused by something other than endometriosis. If this happens frequently, women should see a doctor.
- Being unable to get pregnant.
- Stomach (digestive) problems that may include diarrhea, constipation, bloating or nausea, especially during menstrual periods.
What causes endometriosis?
An exact cause for this condition has yet to be determined, but possible reasons include:
- Retrograde menstruation. This problem involves menstrual blood that contains endometrial cells flowing back through the fallopian tubes and into the pelvic cavity instead of out of the body. These cells stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed during each menstrual cycle.
- Transformation of peritoneal cells. In what’s known as the “induction theory,” experts propose that hormones or immune factors promote transformation of peritoneal cells—cells that line the inner side of your abdomen—into endometrial-like cells.
- Embryonic cell transformation. Hormones such as estrogen may transform embryonic cells—cells in the earliest stages of development—into endometrial-like cell implants during puberty.
- Surgical scar implantation. After surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
- Endometrial cell transport. The blood vessels or tissue fluid (lymphatic) system may transport endometrial cells to other parts of the body.
- Immune system disorder. A problem with the immune system may impede the body’s ability to recognize and destroy endometrial-like tissue growing outside the uterus.
What are the risk factors for endometriosis?
According to experts, several factors can put a woman at greater risk of developing endometriosis, including:
- Never giving birth
- Starting her period at an early age
- Going through menopause at an older age
- Experiencing short menstrual cycles—for instance, less than 27 days—or heavy menstrual periods that last longer than seven days
- Having higher levels of estrogen or greater lifetime exposure to estrogen that her body produces
- Low body mass index
- One or more relatives (mother, aunt or sister) with endometriosis
- Any medical condition that prevents the normal passage of menstrual flow out of the body
- Abnormalities of the reproductive tract.
How is endometriosis diagnosed?
Doctors conduct a pelvic exam, ultrasound, MRI or laparoscopy to confirm whether women have this disorder.
How is endometriosis treated?
Treatment options include medication or surgery, depending on the severity of a woman’s symptoms and whether she wants to become pregnant. Doctors typically recommend that women try conservative approaches before opting for surgery.
For women who aren’t trying to conceive, doctors may recommend hormone therapy, such as hormonal contraceptives (birth control, patches, vaginal rings), progestin therapy and aromatase inhibitors (a class of medicines that reduce the amount of estrogen the body produces).
Individuals trying to become pregnant or experiencing severe pain are given a complete evaluation to check for fertility issues or conditions that can cause pelvic pain. Doctors may refer a woman to a surgeon for a laparoscopy. In this procedure a laparoscope—a thin tube with a video camera—is inserted into a woman’s body via a small incision near the belly button to look for signs of endometrial tissue outside the uterus and other organs. During the procedure, doctors can remove any areas of endometriosis while preserving a woman’s uterus and ovaries.
Many women who opt for the procedure report feeling relief from their pain, but about 20% don’t. In addition, laparoscopic surgery can increase a woman’s chances of getting pregnant. However, each case is different.
Last Reviewed: August 1, 2019